Read, listen and watch
Information & Resources Hub
ARTICLES, PODCASTS, WEBCASTS & MORE
My Journey
LEARN MORE & SIGN UP
The Beacon
READ OUR ONLINE MAGAZINE
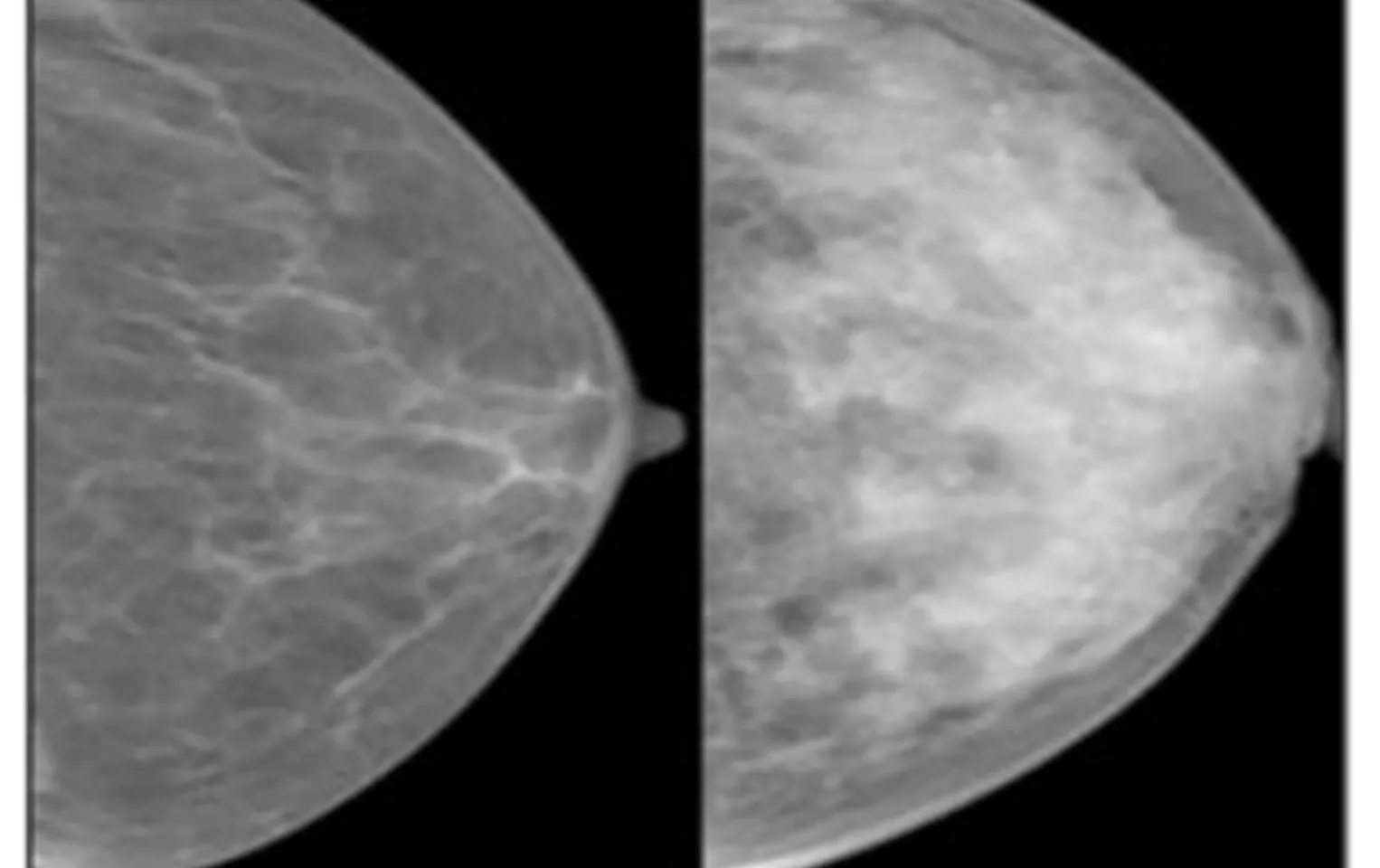
Understanding breast cancer
About breast cancer
TYPES, TREATMENTS & IMPACTS
Breast cancer in Australia
STATISTICS
Find assistance
Call the Helpline
YOUR FIRST CALL
Connect with others
Online Network
VISIT & SIGN UP
Helpful tools and services
Service Finder
FIND SERVICES AND SUPPORT IN YOUR AREA
My Care Kit
LEARN MORE
My Decision
BREAST RECONSTRUCTION DECISION TOOL
News
The Beacon
READ OUR ONLINE MAGAZINE
Event directory
Fundraise with us
Share your experience
Join a consumer group
CONSUMER REPRESENTATIVES, REVIEW & SURVEY GROUP
Partner with us
Donate now
1
2
3
1
2
3
$
Donations over $2.00 are tax-deductible








![[blank]](https://bcna-dxp.azureedge.net/media/en2fczb2/bcna_placeholder_bg.jpg?rxy=0.7593219354887106,0.2881619937694704&width=384&height=240&format=webp&quality=80&rnd=133546802863430000)




![[blank]](https://bcna-dxp.azureedge.net/media/en2fczb2/bcna_placeholder_bg.jpg?rxy=0.7593219354887106,0.2881619937694704&width=64&height=64&format=webp&quality=80&rnd=133546802863430000)
